If you search the web for “root canals” right now, chances are you will get two kinds of results: advertisements for local endodontists (root canal specialists) and articles on the dangers root canal treatment. Multiple pages will come up claiming endodontics are everything from toxic to cancer causing and even DNA altering. Is there any merit to these arguments? In this article, we hope to show you the truth behind root canals- a safe and remarkable treatment that has saved millions of teeth from extraction!
Before we explain the controversy behind endodontics, we need to clarify how the procedure works in general. When a tooth becomes traumatized -be it from decay, physical force or extreme temperatures- the nerve tissue inside can become irritated and dies. This leaves behind a perfect space for bacteria to colonize and form an abscess. The abscess is a collection of bacteria that your immune system has contained and walled off, but cannot eliminate.
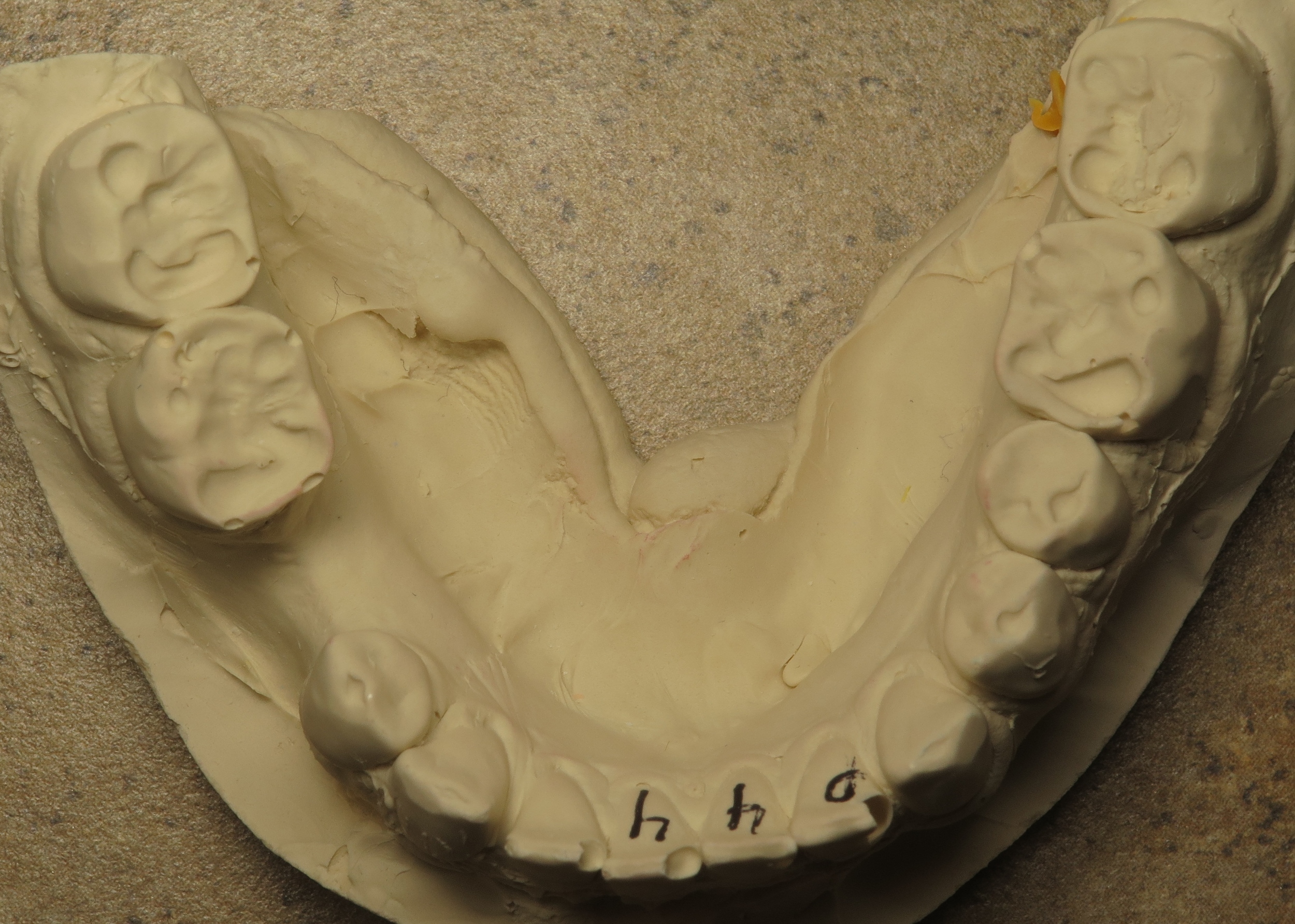
Notice the dark halo around the tooth root (where the arrow is pointing)? That is an abscess that will need to be treated with a root canal.
A root canal tries to interrupt this process before the abscess leads to a dangerous systemic infection or damages the tooth beyond repair. Essentially, the inner tooth structure is cleaned, shaped and sterilized using very specific techniques. After the tooth is completely prepared, the roots are filled with a material called Gutta Percha. Gutta Percha is a natural rubber derived from tree sap that both seals the tooth and resists breakdown. After the endodontic treatment is completed, a crown is placed for increased rigidity and longevity.
A visual guide on how root canals are performed
Many articles that criticize endodontic treatment quote studies that were performed by Dr. Weston Price in the 1920’s. His research indicated that bacteria from incompletely sealed root canals could spread out to the rest of the body and cause systemic problems like arthritis and cancer. These conclusions were quickly disproved, as his data was obtained using outdated and inaccurate scientific methods. Current research shows no correlation between root canal treatment and increased risk for any disease. It is important to remember that the end goal of endodontics is to lower the bacterial load from infection, so that your immune system can naturally eliminate any residual microorganisms. In this sense, endodontics seek to work with your body, not against it!
Still, many internet blogs insist that root canals can cause cancer. A commonly quoted statistic is that 97% of terminal cancer patients have at least one root canaled tooth. First, it is unclear what scientific study this number actually originated from. Secondly, even if there is a correlation, there is no causation between root canals and cancer. It would be equally (in)valid to say that cancer causes root canals- a truly absurd notion. Finally, this statistic is almost certainly false. A 2013 study by the Journal of the American Medical Association found that patients with root canals actually had a 45% lower cancer risk (again, this describes correlation and not necessarily causation).
Overall, we can see that the majority of the anti-root canal argument relies on 90 year old disproven research, conjecture and anecdotal evidence. In contrast, peer-reviewed scientific research on endodontic treatment has continuously demonstrated that root canal therapy is safe, effective and highly successful. If you have further questions on root canals and why they are great treatment options, please give our office a call. We are always excited to keep our patients informed and knowledgeable on the best practices in dentistry!